Why all the insistence that as a patient you should set up your patient portal? You may be thinking that patient portals are cumbersome, complicated and technology is just too difficult to set up. Let me assure you that it does take effort, but there are many benefits to engaging with your patient portal.
At Scottsdale Mental Health & Wellness Institute, we have integrated the patient portal into our patient care. We assist our patients with setting up their portal and walk them through the initial setup of the portal. We help patients gain access to all the features and benefits available. The portal serves many functions including providing options for communication with your providers, information about upcoming appointments, the ability to complete documentation, and features that can improve your mental health functioning.
We utilize the patient portal for the entire admission paperwork process which is done through an e-signature application that gets imported directly into your chart once completed. Our admissions staff provides additional options for those who don’t have access to computer equipment or who have difficulty managing technology. We have patients complete intake paperwork in person, have patients fax documents to the practice, and send the documents in an attachment via email. We then upload all those documents into your chart.
Once your Patient Portal is set up, you have secure access to information about your care. The Patient Portal allows you to directly communicate through the messaging feature with your provider. If you are seeing multiple providers then the additional provider can start a message with you and you can communicate with your entire team.
Prior to your initial appointment, our team will send you what is called “treatment measures”. These measures are tools to help your provider evaluate your emotional condition and understand your level of functioning prior to your appointment. The measures show up in your portal two days before your session. When completed the measures are imported into your chart so your provider can review your status. Measures are very helpful to your provider because they can review your status before they even see you in session. These measures save your provider time so they can dedicate more time to listen to your issues and concerns. Over time the practice can also track progress with your emotional/psychological condition by looking at the results of your measures. So please if your portal is set up, keep an eye out for the emails that inform you that you have measures to complete. Measures are also ongoing while you are in treatment.
At SMHWI, we are rolling out many other features of the portal so patients can benefit more from using the Patient Portal which is directly linked to your Electronic Health Record. Our goal is to provide solutions for our patients which improve patient care and improve patient functioning. We understand that many people struggle with technology and we want you to know that we will support you with any technical limitations you may have. We hope you benefit from the Patient Portal in the future.
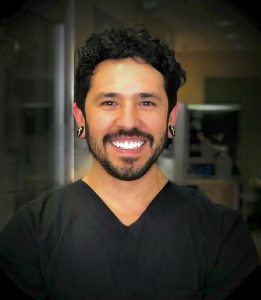
Author: Patrick Mingey, Director of Marketing
Patrick brings unique and varied skills to his position as Director of Marketing. His background includes 15 years as an addiction therapist and 41 years of personal recovery. He has dedicated his life to helping others and has worked with thousands of people who suffer from addiction and mental health disorders. He is passionate about making a difference in the lives of those he interacts with. Patrick has extensive experience in marketing and previously ran his own marketing company in which he provided graphic design, website development, and content marketing. He is very excited to offer not only his marketing expertise to Scottsdale Mental Health & Wellness Institute, but also offer his passion for helping others.